How I Caught My Body’s Red Flags Early with Acupuncture and Massage
I used to ignore little aches—tight shoulders, morning stiffness, restless sleep—until they screamed for attention. That changed when I started acupuncture and massage not just for relief, but as a wellness radar. These ancient practices helped me tune into my body’s subtle signals, revealing imbalances long before serious issues surfaced. It’s not magic—it’s mindfulness backed by tradition. If you’ve ever wondered how to stay ahead of illness, this is where to start. What began as occasional visits for stress relief evolved into a consistent practice of listening, learning, and responding to my body in ways I never thought possible. Today, I don’t wait for pain to act. Instead, I pay attention to the whispers—the slight tension in my neck, the way my lower back feels after sitting too long, the quality of my breath during quiet moments. These small cues, once dismissed, now guide my health choices with surprising clarity.
Listening to the Body’s Whisper: Why Early Signals Matter
Most women in their 30s to 50s are no strangers to fatigue, stress, or the occasional ache. Juggling family, work, and personal responsibilities often means putting physical discomfort on the back burner. A stiff neck after a long day? Normal. Occasional headaches? Probably just dehydration. But what if these weren’t just passing inconveniences, but early messages from the body? The truth is, mild symptoms like muscle tightness, joint stiffness, or disrupted sleep are not always signs of overwork—they can be the first indicators of deeper imbalances. Inflammation, poor circulation, nerve irritation, or postural strain often begin subtly, long before they develop into diagnosable conditions. The problem is, modern medicine typically waits for symptoms to become severe before intervening. By then, the body has already been struggling in silence for months, even years.
Acupuncture and massage offer a different approach—one that values sensitivity over severity. These therapies don’t just treat pain; they help uncover its roots. When a skilled practitioner works with your body, they’re not only applying techniques—they’re observing how your tissues respond. A muscle that resists pressure, a point that flares with sensation when touched, or an area that feels unusually cool or warm—all of these are clues. In traditional Chinese medicine, such reactions are seen as disruptions in the flow of qi, or vital energy, along meridians that correspond to organ systems and physiological functions. From a Western perspective, these same areas may indicate trigger points, fascial restrictions, or neurological sensitivities. Either way, the body is communicating. The real power lies in learning to listen before the message becomes a crisis.
Consider the case of chronic shoulder tension. Many women carry stress in their upper back and neck, often due to prolonged sitting, emotional strain, or repetitive movements like driving or typing. Left unaddressed, this tension can lead to headaches, reduced range of motion, or even nerve compression in the cervical spine. But with regular bodywork, such patterns can be caught early. A massage therapist might notice that one trapezius muscle is significantly harder than the other, suggesting asymmetry and possible compensation from another area. An acupuncturist might find heightened sensitivity at points linked to the gallbladder or liver meridians, which in traditional terms relate to stress processing and muscle health. These findings don’t mean disease is present—they mean the body is adapting, and adaptation has limits. Recognizing these early signs allows for timely intervention, potentially avoiding more invasive treatments down the road.
Acupuncture: More Than Pain Relief—A Detection Tool
Acupuncture is often misunderstood as a last resort for chronic pain or a niche alternative for those who’ve exhausted conventional options. But for many, it serves a far more proactive role—one of detection and prevention. When fine, sterile needles are inserted at specific points on the body, they do more than stimulate healing; they test the body’s responsiveness. A skilled practitioner pays close attention to how tissues react: Does a needle elicit a twitch? Is there referred sensation down an arm or leg? Does the area feel unusually tender compared to previous sessions? These responses are not random—they are meaningful indicators of underlying function.
For example, consistent tenderness at Liv3 (Taichong), a point on the foot associated with the liver meridian, may suggest emotional stress, hormonal fluctuations, or even early signs of metabolic imbalance, even when blood tests appear normal. Similarly, sensitivity at ST36 (Zusanli), located below the knee, can reflect digestive inefficiency or immune system fatigue. These points are not diagnostic in isolation, but when tracked over time, they form a pattern that reveals how the body is coping. This is especially valuable for women navigating perimenopause, when hormonal shifts can create vague symptoms like fatigue, mood swings, or sleep disturbances that are hard to quantify through standard testing.
Modern research supports the idea that acupuncture influences the nervous system in measurable ways. Studies have shown that needle stimulation can modulate inflammation, regulate cortisol levels, and improve autonomic balance—shifting the body from a stressed “fight-or-flight” state to a calmer “rest-and-digest” mode. But beyond these benefits, the treatment itself provides feedback. If a session leads to unexpected changes—like improved digestion, clearer thinking, or deeper sleep—it may indicate that a long-standing imbalance was quietly affecting overall function. In this way, acupuncture becomes a form of body literacy, helping individuals recognize how different systems are interconnected. It’s not about chasing symptoms, but about understanding the whole picture.
Massage as a Diagnostic Experience
Massage is often viewed as a luxury—a treat for tired muscles or a reward after a busy week. But when performed by a trained therapist, it is also a powerful assessment tool. Unlike imaging tests that capture a static image, massage offers dynamic, real-time evaluation of the body’s soft tissues. As hands move across the back, legs, or arms, they detect variations in muscle tone, temperature, texture, and mobility. A skilled therapist can feel the difference between healthy, pliable tissue and areas of fibrosis, adhesion, or chronic guarding—changes that may not show up on an MRI but can significantly impact movement and comfort.
Take, for instance, the gluteal muscles. One side may feel significantly denser or cooler than the other, suggesting a pelvic imbalance that could contribute to hip or knee pain over time. Or consider the fascia along the spine—when it feels tight and restricted, it may indicate postural strain from prolonged sitting or emotional tension held in the body. Scar tissue from past injuries, even minor ones, can also be detected through touch, revealing areas where movement is limited and circulation may be compromised. These findings are not just for correction—they are data points that help build a functional map of the body.
Over time, regular massage creates a baseline. Just as a doctor tracks blood pressure or cholesterol levels, a therapist can track changes in tissue quality, symmetry, and response to pressure. When a new knot appears, or an old area becomes more sensitive, it signals that something has shifted. This could be due to a change in activity level, emotional stress, or even dietary habits. The beauty of this hands-on monitoring is its immediacy. There’s no waiting for test results or insurance approvals—feedback is available in the moment. For women who are attuned to their bodies, this can be a powerful way to stay ahead of issues before they become debilitating.
The Science Behind Sensory Feedback
While acupuncture and massage are rooted in centuries-old traditions, modern science is increasingly validating their role in health monitoring. Research in the field of myofascial medicine has shown that restrictions in connective tissue can affect nerve conduction, blood flow, and joint mechanics, contributing to chronic pain and dysfunction. A 2020 review published in the Journal of Bodywork and Movement Therapies highlighted that myofascial release techniques can lead to measurable improvements in range of motion and pain reduction, suggesting that tissue changes occur well before structural damage becomes visible on scans.
Similarly, studies on acupuncture have demonstrated its ability to influence biomarkers of inflammation, such as interleukin-6 and C-reactive protein. One clinical trial found that regular acupuncture sessions over eight weeks led to significant reductions in inflammatory markers among participants with chronic low back pain. These changes weren’t just linked to pain relief—they correlated with improved energy levels, mood, and sleep quality. This suggests that the body’s response to treatment is not merely symptomatic but reflective of deeper physiological shifts.
The nervous system plays a central role in this process. Both acupuncture and massage stimulate sensory nerves in the skin and muscles, sending signals to the brain that can reset autonomic function. This is why many people report feeling calmer, more focused, or even emotionally lighter after a session. These responses are not imagined—they are neurologically grounded. When the parasympathetic nervous system is activated, heart rate slows, digestion improves, and immune function strengthens. Over time, paying attention to these shifts builds a personal health narrative. If improved sleep follows a particular acupuncture point being stimulated, or if shoulder tension eases after a specific massage technique, it creates a feedback loop that enhances body awareness and informs future care decisions.
Building a Prevention Routine
Incorporating acupuncture and massage into a wellness routine is not about indulgence—it’s about strategy. For women managing households, careers, and aging parents, self-care is often seen as optional. But preventive bodywork is not a luxury; it’s a long-term investment in health resilience. Starting with monthly sessions allows for consistent tracking of physical and emotional patterns. Over time, these visits become more than treatment—they become check-ins, much like dental cleanings or annual physicals.
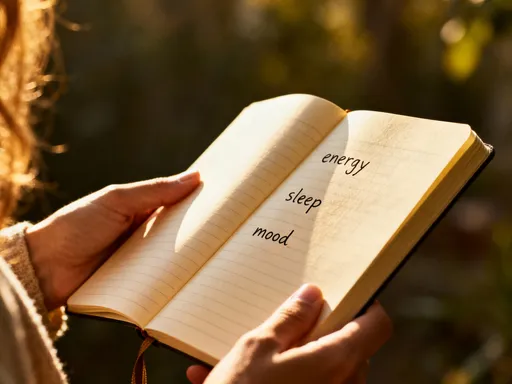
To maximize the benefits, it helps to pair professional care with mindful self-assessment. Simple practices—like noticing how your body feels upon waking, checking your posture in the mirror, or rating your energy levels on a scale of one to ten—can reveal trends. Keeping a brief journal to record physical sensations, sleep quality, and emotional state can deepen awareness. When a pattern emerges—say, increased lower back tension during stressful work weeks—it becomes easier to take proactive steps, such as scheduling a session or adjusting daily habits.
Consistency is key. Just as brushing your teeth daily prevents cavities, regular bodywork helps maintain tissue health and detect changes early. Some women choose to increase frequency during transitional periods, such as seasonal shifts or perimenopausal changes, when the body may need extra support. Others use it as a reset after travel, injury recovery, or periods of high stress. The goal is not perfection, but presence—staying connected to your body’s rhythm so you can respond with care, not crisis.
When to Seek Professional Medical Advice
It’s important to emphasize that acupuncture and massage are complementary practices, not replacements for medical diagnosis. While they offer valuable insights, they do not substitute for clinical testing or physician evaluation. Any persistent or worsening symptom—such as unexplained pain, numbness, tingling, fatigue, or changes in bowel or bladder function—should be discussed with a licensed healthcare provider. These therapies are best used as early warning systems, not final answers.
Think of it this way: acupuncture and massage may detect the first whisper of imbalance, but doctors provide the full conversation. If a therapist notices significant asymmetry or an area of concern, they should encourage you to seek further evaluation. Similarly, if acupuncture reveals consistent patterns that suggest organ system stress, it’s wise to consult your physician and possibly run lab tests. Always work with licensed practitioners who understand the boundaries of their scope and are willing to collaborate with your medical team. Sharing your treatment experiences with your doctor can lead to a more integrated, comprehensive approach to care.
A Lifelong Commitment to Body Awareness
True wellness is not measured by the absence of disease, but by the presence of awareness. Acupuncture and massage have taught me to honor my body’s language—not as a source of inconvenience, but as a guide. The small investments I make in listening—through regular sessions, mindful movement, and honest self-reflection—have paid long-term dividends in energy, mobility, and peace of mind. I no longer wait for pain to demand attention. Instead, I tune in early, respond with care, and move through life with greater clarity and control.
This is not a cure-all, nor a substitute for medical science. It is, however, a powerful piece of a smarter, more responsive health journey. For women who carry the weight of responsibility and the quiet burden of self-neglect, this shift can be transformative. By learning to read the subtle signals—the tightness, the fatigue, the restless night—you gain time. Time to act, to heal, to prevent. You gain understanding of how your body truly works, and how small changes can lead to lasting well-being. In a world that often moves too fast, this practice is a quiet rebellion—a commitment to listening, learning, and living with intention.